THE FIRST STEP TO GETTING TESTED

When you are suspected of obstructive sleep apnea or other sleep disorders, the first step is seeing a sleep medicine specialist who can access your symptoms, medical history, lifestyle factors including sleep patterns, and conduct a questionnaire, which includes patient medical history, family history, social history, sleep history and the Epworth Sleepiness Scale (ESS).
The ESS is a questionnaire that consists of eight questions that ask the subject to rate their likelihood of falling asleep in common situations, such as sitting and talking to someone, or being in a car while stopped in traffic.
THE SECOND STEP TO GETTING TESTED
When all of the above data is considered and the patient is evaluated by a sleep physician, then testing is the second step. Innovative and state-of-the-art testing leads to an accurate diagnosis. And diagnosis is an essential step before a treatment plan can be developed specific the patient’s needs.
Accurate sleep testing usually leads to accurate diagnoses because it provides essential data for medical professionals to make confident treatment decisions. Accurate and timely test results also provide clear indicators that can be communicated to the patient, increasing their confidence in the treatment plan, and assurance of excellent patient care. When a patient feels confident of the diagnosis, adherence to the treatment increases exponentially.
THE THIRD STEP TO TREATMENT
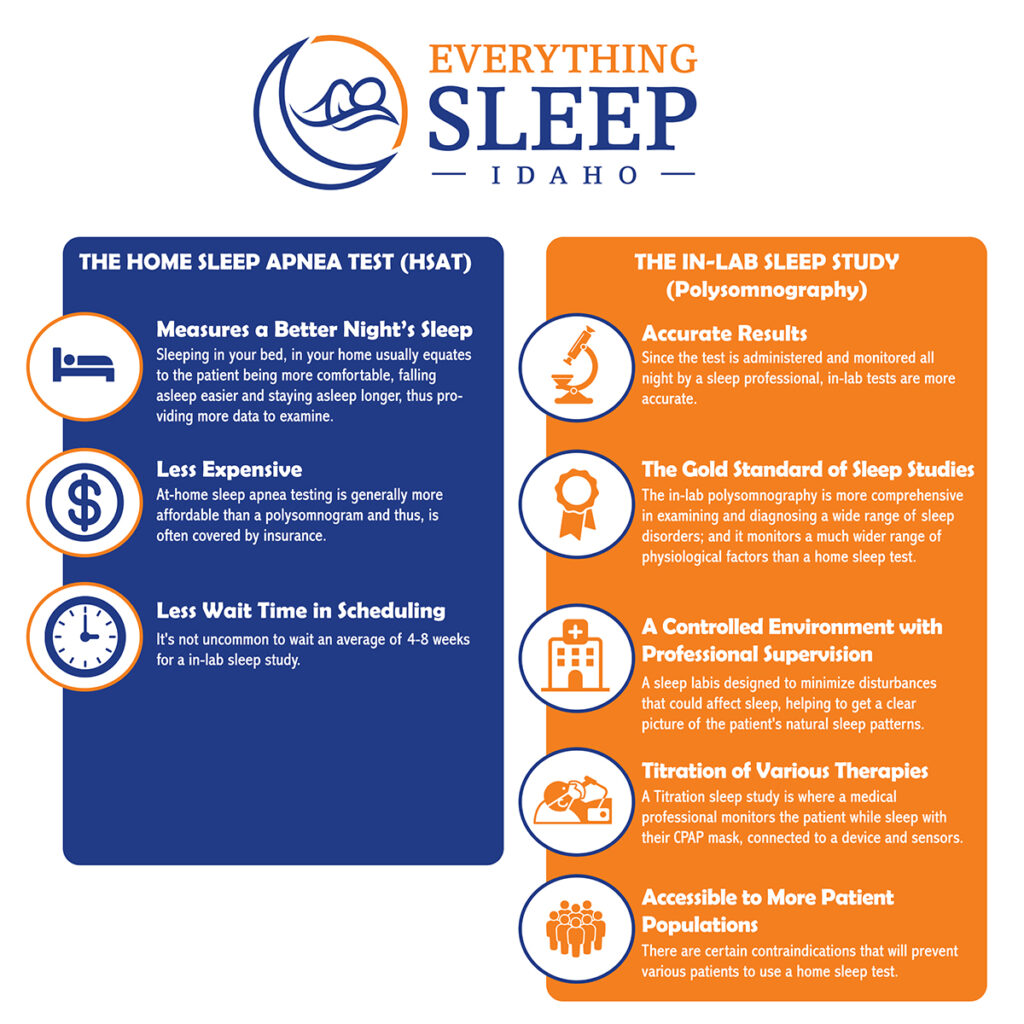
Once a healthcare professional or sleep physician decides a sleep test is needed, they will decide which type of sleep study to order. The choice is between a Home Sleep Test (HSAT) or a Polysomnography Test at a sleep clinic or hospital; and both are now widely available. What is the process of each test and how does it work? Which test is more accurate, more comprehensive, or less expensive? What test records more physiological signals during sleep? What are the pros and cons of each type of sleep study? How does the patients’ demographics or comorbidities come into the decision of which test they can undergo?
THE HOME SLEEP APNEA TEST (HSAT)
What is a HSAT?

A home sleep apnea test is a very simplified breathing monitor that tracks your breathing, oxygen levels, and breathing effort while worn. A home sleep study evaluates a patient for sleep apnea, by monitoring breathing parameters, but not the sleep itself. It will measure pauses in and absence of breathing, how much effort it takes to breathe and whether your breathing is deep or shallow.
How does it work? The HSAT uses sensors that include a small probe that goes over your finger to measure oxygen levels and a mask that is held in place around your ears, with a nasal cannula. A nasal cannula is a thin, flexible tube to measure airflow into and out of the nose while a person breathes. The cannula is placed in the nostrils and plugs into a small data monitor worn on the chest. More sensors go onto your abdomen and chest to measure when your body rises and falls as you breathe.
What are the benefits of HSAT?
Measures a Better Night’s Sleep
An HSAT often sounds more appealing to most patients, as it’s obvious that sleeping at home is preferable over sleeping in a new environment. And science proves that a better nights’ sleep happens at home with the study of the “first-night effect”.
Many patients experience what sleep experts call the “first-night effect” which means that people tend to have impaired or worse sleep the first night they spend in an unfamiliar environment or setting. The “first-night effect” initially was discovered by studies in sleep clinics and it may not improve during consecutive nights. And the quality of environment does not necessarily affect the “first-night effect”, as further research found that sleep quality was reduced even in a warm and inviting setting, whether at a sleep clinic or a four-star spa resort. (The National Center of Biotechnology)
Another benefit is additional comfort, as home tests are minimally invasive (with less testing equipment attached to the body) in a non-intrusive environment (your home), which both contribute to improved sleep quality. Sleeping in your bed, in your home usually equates to the patient being more comfortable, falling asleep easier and staying asleep longer, thus providing more data to examine.
What other advantages does a HSAT Test provide?
Less Expensive
At-home sleep apnea testing is generally more affordable than a polysomnogram and thus, is often covered by insurance. What are the price differences? Considering various health insurance coverages, whether in or out-of-network, in-lab sleep test costs can range from $4,500 and upwards of $10,000[MR1] . Most healthcare providers will confirm insurance coverage first before scheduling a sleep study, and in most cases, the out-of-pocket patient cost is typically much lower that the medical bill. In stark contrast, a home sleep test usually range below $450, regardless of your insurance policy.
Less Wait Time in Scheduling
Recent Statistics:
- From 2% to 9% of all adults have OSA – Robert L Owens, MD, MSD Manuals, August 2024
- It’s four times more common in men; and seven more times more common who are obese. – AASM
- The HypnoLaus found 23.4% of women and 49.7% of men showed signs of moderate-to-severe sleep-disordered breathing. – NIH
- Women are also much more likely to develop OSA during and after menopause. – NIH
Because the symptoms and the risks of sleep disorders are more recognized and better understood by the health care industry, consequentially sleep labs are in higher demand. Therefore, conducting an at-home sleep study (which became increasingly popular during the pandemic), has reduced the demand on sleep labs and sleep centers. As a result, they have shortened wait times for patients to get tested.
It’s not uncommon to wait an average of 4-8 weeks for a in-lab sleep study. In that time, it could deter many patients to get tested at all, but it’s recommended to either wait or ‘shop around’ for another facility for those who have been prescribed and genuinely need a lab sleep test.
Another advantage over home sleep tests is that results also can be provided quicker. A lab sleep test simply has more data to be reviewed and analyzed than a home test. Therefore, you can get results in less than a week, sometimes even a few days.
Therefore, we have discussed the primary three benefits (Comfort, Affordability and Less Wait) of a Home Sleep Test, which also have provided the three primary cons of a Lab Sleep Test. So now let’s discuss the five pros of a Lab Sleep test, which in turn are also the cons of a Home Sleep test.
THE IN-LAB SLEEP STUDY (Polysomnography)

What is a Polysomnography?
This sleep study takes place in a hospital, sleep lab or sleep center, administered by a Sleep Technician or Respiratory Therapist, and records many physiological signals during sleep. During the test, the patient is connected to sensors and electrodes that monitor the following data signals:
- Brain activity and brain waves
- Heart rate and rhythm (ECG)
- Breathing effort, airflow, oxygen levels, and carbon dioxide levels
- Eye movement frequency and speed
- Leg movements also known as leg electromyogram (EMG)
- Oxygen saturation in the blood
- Sleep latency
- Sleep duration
- Sleep efficiency
How does it work? After the patient arrives, when they are ready for bed, the technician will place the sensors to the scalp, temples, chest and legs using a mild adhesive such as glue or tape. The sensors’ wires are connected to a computer but are long enough to let you move around in bed. A small clip is also placed on your finger or ear to measure the level of oxygen in your blood.
After the test, a doctor will review the results and develop a treatment. A normal AHI score is less than 5, while scores of 5–15, 15–30, and greater than 30 indicates a mild, moderate, or severe sleep apnea.
What are the benefits of a polysomnography?
Accurate Results
Since the test is administered and monitored all night by a sleep professional, in-lab tests are more accurate because the sensors have been placed correctly, the equipment is tested and set up properly, and the all-night monitoring is handled by an experienced and licensed sleep technologists. The margin of error and anomalies increase with home sleep studies as the patient is placing the sensors, and setting up the equipment, without a professional monitoring the data throughout the night.
The Gold Standard of Sleep Studies

The in-lab polysomnography is considered the Gold Standard of sleep studies because is more comprehensive in examining and diagnosing a wide range of sleep disorders; and it monitors a much wider range of physiological factors than a home sleep test. Home sleep studies can be used specifically for diagnosing moderate to severe obstructive sleep apnea, and that’s it.
“In lab tests can accurately measure total sleep-time, which is generally at best, estimated using an Ambulatory Polysomnography (PSG). Being that most indexes for sleep, like the AHI, are based on time slept. The inaccurate TST really affects the accuracy of ambulatory polysomnography. Ambulatory PSG has a false negative rate for diagnosing OSA of up to 15%.” – Dr. Mark Rasmus, M.D.
The test results are more comprehensive as there are many more physiological effects being monitored, so the sleep physician has a fuller understanding of the patient’s sleep stages, eye movements, eye activity, and oxygen saturation levels. Therefore, diagnoses are more specific because the in-lab study tests for a wide variety of sleep disorders including sleep apnea (obstructive and central), narcolepsy, periodic limb movement disorder, restless leg syndrome, insomnia, seizures, sleep paralysis, nocturnal panic attacks, night terrors or hallucinations, and other disruptive sleep disorders.
A Controlled Environment with Professional Supervision

The sleep environment at a sleep lab is designed to minimize noise, light, and other disturbances that could affect sleep, helping to get a clear picture of the patient’s natural sleep patterns. At Everything Sleep Idaho, our sleep clinic is equipped with state-of-the-art monitoring equipment and facilities to ensure accurate diagnosis and effective treatment. This includes specialized sleep monitoring devices, comfortable sleep rooms designed to simulate a home-like environment, and advanced technology for data analysis and interpretation.
In sleep testing facilities, sleep technicians monitor the study in real-time, allowing them to adjust sensors or equipment, if needed, to ensure accurate data collection. With real-time monitoring, the technicians can respond immediately when significant issues arise, such as severe oxygen desaturation. At our sleep clinic, we are staffed with healthcare professionals specializing in sleep medicine including sleep physicians and board-certified sleep technologists, all who oversee the diagnosis and treatment of sleep disorders.
Titration of Various Therapies
For any patients who are suspected of having OSA, the in-lab test allows for CPAP (Continuous Positive Airway Pressure) titration. Utilizing the CPAP mask and device during the sleep study, allows for the technician to determine the optimal pressure settings. Other sleep-related therapies can be tested as well, including supplemental oxygen or bilevel positive airway pressure (BiPAP).
What is a CPAP Titration study? It’s a sleep study is where a medical professional monitors the patient while sleep with their CPAP mask, connected to a device and sensors. The technician can calibrate a CPAP machine to the correct air pressure for an individual’s sleep-related breathing disorder, by gradually increasing air pressure and carefully monitoring the effects on breathing, body movements, and sleep quality.
Accessible to More Patient Populations
There are certain contraindications that will prevent various patients to use a home sleep test, including patients under 18 years of age, patients with cardiac or pulmonary issues, congestive heart failure, COPD, moderate to severe cardiac disease, moderate to severe pulmonary disease, or progressive neuromuscular disorders, those dependent on supplemental oxygen, and those who have recently had a stroke.
In these cases, an in-lab polysomnographic study will be ordered for a medical professional to monitor and evaluate the patient throughout the study to ensure there is no potential risk to the patient’s health.
In Conclusion,
While we have examined the pros and cons of each type of sleep test, whether at home or in lab, it is the physician who will determine which test is most appropriate and medically necessary for the patient and the suspected diagnoses. In a future blog, we will discuss the differences when it comes to preparation of the test, steps for setup for a home test specifically, and what happens after the test when it comes to evaluating the data and developing a customized treatment plan.
Our approach to Sleep Medicine is focused on the importance of quality sleep and sleep hygiene. Quality sleep is essential for overall health and well-being. Adequate sleep contributes to physical health, mental health, cognitive function, immune function, and emotional regulation. Let’s get started on a better night’s sleep!